A new single-center study has shown that the catheterization laboratory (CCL) activation in response to a prehospital ECG interpreted as ST-segment elevation myocardial infarction (STEMI) can be frequently canceled which represents an economic burden and affects the patient satisfaction negatively.
The study that was recently published in Circulation showed that 65% of the cases of CCL activation at Cedars Sinai Medical Center (CSMC) in Los Angeles were canceled in the period from January 1, 2012, to December 31, 2014. The patients who had their CCL activation canceled (CCLx) were compared to the patients who had emergent coronary angiography (EA) and interestingly, differences were found between the patient criteria of the two groups and their clinical outcomes.
Dr. David Lange, The principal investigator, and the interventional cardiologist, Kaiser Permanente Medical Group says, “To our knowledge, this is the first study to examine the reasons for CCL cancellation and the clinical outcomes of CCL cancellation patients.”
Differences between the groups
According to the study, CCLx is more likely to occur with females, older patients, those with a history of coronary artery disease, those who had coronary artery bypass grafting before (CABG), or had paced rhythm.
Regarding the outcomes, cardiac death was significantly higher in the EA patients while all-cause mortality was more common among the CCLx group after adjustment for other factors that may affect the survival such as smoking history and the presence of signs of congestive heart failure.
It was also found that the initial and peak troponin levels in the CCLx group were lower than that of the EA group. Additionally, when comparing the proportion of patients from the CCLx group who had coronary angiography during their index hospitalization to those of the EA group, it was found that CCLx patients were more likely to have either no culprit vessel or multiple culprit vessels.

“To our knowledge, this is the first study to examine the reasons for CCL cancellation and the clinical outcomes of CCL cancellation patients.” -Dr. David Lange
“We concluded that pre-hospital ECG without over-reading or transmission may lead to frequent CCL cancellations and that these subjects differ with regards to age, gender, risk factors, and co-morbidities. However, CCL-cancellation patients represent a high-risk population, with similar short and long-term mortality compared to patients who receive emergent coronary angiography,” Dr. Lange adds.
Reasons for CCLx and inappropriate CCLx
The reasons for CCLx were also investigated in the study. The presence of right bundle branch block (interpreted as myocardial infarction), poor quality of the prehospital ECG, and non STEMI ST-segment changes were the top three reasons representing about 60% of the cases.
The study also reported the rate of inappropriate CCLx (0.7%), defined as canceled activation of the catheterization lab despite the patient having the criteria for appropriate activation (typical chest pain, ECG showing ST elevation, and positive cardiac enzymes).
Dr. Lange adds, ” I would emphasize that the CCL cancellations were, for the most part, appropriate, as there was a < 1% rate of ‘inappropriate’ cancellation on independent review. Secondly, CCL cancellation patients are a very sick patient population with similar all-cause mortality at 1 year to STEMI patients. As such, triage to a tertiary care facility for stabilization and treatment is probably an appropriate care pathway.”
The literature discussing this topic showed a wide range of CCLx rate (from 5% to 60%). This variability in CCLx rate was due to the discrepancy in defining the appropriate CCL activation among the studies. Additionally, the reasons for CCLx and the clinical outcomes of the patients were not studied well.
Application to practice
When asked about the application of these findings into clinical practice, Dr. Lange answered “As a result of these findings we developed a novel CCL team activation algorithm (shown below) which mirrors our Trauma team activation. In this new system, all pre-hospital ECGs are reviewed by the Emergency Department physician prior to the patients’ arrival and are triaged into two different pathways. A ‘STEMI 100’ is a clear-cut STEMI that meets criteria for CCL activation and is triaged immediately to the CCL, with minimal evaluation in the emergency department. A ‘STEMI 200’ is a possible STEMI patient that requires medical stabilization and/or further evaluation in the emergency department by the cardiology team and the emergency medicine team prior to CCL team activation. A STEMI 200 can be ‘elevated’ to a STEMI 100 and triaged to the CCL immediately.”
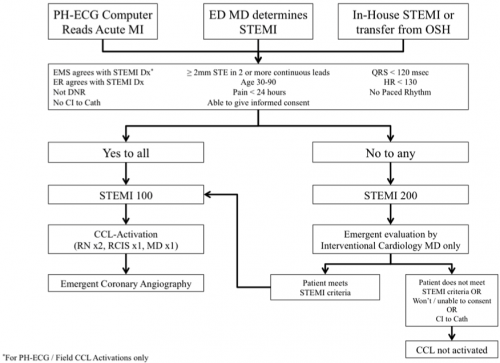
Courtesy of Dr. David Lange
Source: https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.117.004464



Leave a Reply
You must be logged in to post a comment.